BACKGROUND
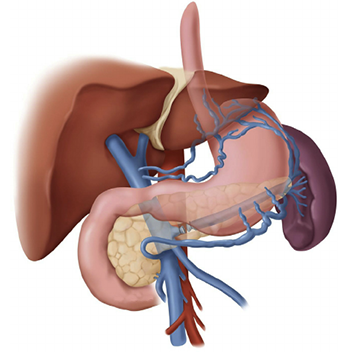
Portal hypertension is an increase in the blood pressure within a system of veins called the portal venous system. Veins coming from the stomach, intestine, spleen, and pancreas merge into the portal vein, which then branches into smaller vessels and travels through the liver. If the vessels in the liver are blocked due to liver damage, blood cannot flow properly through the liver. As a result, high pressure in the portal system develops. This increased pressure in the portal vein may lead to the development of large, swollen veins (varices) within the esophagus, stomach, rectum, or umbilical area (belly button). Varices can rupture and bleed, resulting in potentially life-threatening complications.
DISEASE OCCURRENCE IN POPULATION
Portal hypertension is a frequent manifestation of liver cirrhosis. According to the National Institute on Alcohol Abuse and Alcoholism (NIAAA), liver cirrhosis accounted for almost 30,000 deaths in the United States in 2007, making it the 12th leading cause of US deaths. The frequency of gastroesophageal varices directly correlates with the severity of the liver disease from 40% in Child class A to 85% in Child class C. Unfortunately, total population-based prevalence data for portal hypertension in Pakistan is not available. In a small study conducted at Liaquat Medical College it was found that the prevalence of Portal hypertension was 42% among cirrhotic patients.
RISK FACTORS
- Variceal size – The larger the varix, the higher the risk of rupture and bleeding; however, patients may bleed from small varices too.
- The presence of endoscopic red color signs (e.g. red wale markings, cherry red spots)
- Child B or C classification, especially the presence of ascites, increases the risk of hemorrhage
- Active alcohol intake in patients with chronic, alcohol-related liver diseases
- Local changes in the distal esophagus (e.g. gastroesophageal reflux) – These have been postulated to increase the risk of variceal hemorrhage.
Bacterial infection – A well-documented association exists between variceal hemorrhage and bacterial infections, and this may represent a causal relationship.
SIGN AND SYMPTOMS
The onset of portal hypertension may not always be associated with specific symptoms that identify what is happening in the liver. But if you have liver disease that leads to cirrhosis, the chance of developing portal hypertension is high.
The main symptoms and complications of portal hypertension include:
- Gastrointestinal bleeding: Black, tarry stools or blood in the stools; or vomiting of blood due to the spontaneous rupture and bleeding from varices.
- Ascites: An accumulation of fluid in the abdomen.
- Encephalopathy: Confusion and forgetfulness caused by poor liver function and the diversion of blood flow away from your liver.
- Reduced levels of platelets or decreased white blood cell count.
DIAGNOSTIC TESTS
Usually, doctors make the diagnosis of portal hypertension based on the presence of ascites or of dilated veins or varices as seen during a physical exam of the abdomen or the anus. Various lab tests, X-ray tests, and endoscopic exams may also be used.
Before receiving either of the procedures, you will have the following tests to determine the extent and severity of your portal hypertension:
- Evaluation of your medical history.
- A physical examination.
- Blood tests.
- Angiogram.
- Ultrasound.
- Endoscopy.
TREATMENT OPTIONS
The effects of portal hypertension can be managed through diet, medications, endoscopic therapy, surgery, or radiology. Once the bleeding episode has been stabilized, treatment options are prescribed based on the severity of the symptoms and on how well your liver is functioning.
First level of treatment
When you are first diagnosed with variceal bleeding, you may be treated with endoscopic therapy or medications. Dietary and lifestyle changes are also important.
Endoscopic therapy consists of either sclerotherapy or banding. Sclerotherapy is a procedure performed by a gastroenterologist in which a solution is injected into the bleeding varices to stop or control the risk of bleeding. Banding is a procedure in which a gastroenterologist uses rubber bands to block the blood supply to each varix (enlarged vein).
Medications such as beta blockers or nitrates may be prescribed alone or in combination with endoscopic therapy to reduce the pressure in your varices and further reduce the risk of recurrent bleeding.
Medications such as propranolol and isosorbide may be prescribed to lower the pressure in the portal vein and reduce the risk of recurrent bleeding.
The drug lactulose can help treat confusion and other mental changes associated with encephalopathy. This medication has the ability to increase the amount of bowel movements you will have per day.
Second level of treatment
If the first level of treatment does not successfully control your variceal bleeding, you may require one of the following decompression procedures to reduce the pressure in these veins.
- Transjugular intrahepatic portosystemic shunt (TIPS): A radiological procedure in which a stent (a tubular device) is placed in the middle of the liver.
- Distal splenorenal shunt (DSRS): A surgical procedure that connects the splenic vein to the left kidney vein in order to reduce pressure in your varices and control bleeding.
Other treatment procedures for portal hypertension:
- Liver transplant is done in cases of end-stage liver disease.
- Devascularization is a surgical procedure that removes the bleeding varices. This procedure is done when a TIPS or a surgical shunt is not possible or is unsuccessful in controlling the bleeding.
The accumulation of fluid in the abdomen (called ascites) sometimes needs to be directly removed. This procedure is called paracentesis.
PRECAUTIONS
Maintaining good nutritional habits and keeping a healthy lifestyle may help patient avoid portal hypertension.
- Alcohol intake should strongly be discouraged, especially in patients with alcoholic cirrhosis. Available resources for alcohol rehabilitation should be provided, along with any prophylaxis for alcohol withdrawal symptoms, when indicated.
- Do not take any over-the-counter or prescription drugs or herbal medicines without first consulting your doctor or nurse. (Some medications may make liver disease worse.)
- Follow the dietary guidelines given by your health care provider, including eating a low-sodium (salt) diet. You will probably be required to consume no more than 2 grams of sodium per day. Reduced protein intake may be required if confusion is a symptom. A dietitian can create a meal plan for you.
Unless contraindicated, all patients with esophageal varices should take beta-blockers to reduce the risk of bleeding. Patients should also be educated about the adverse effects of beta-blockers and the possible risks of their abrupt discontinuation.
Advise patients who have ascites of the risk of spontaneous bacterial peritonitis during an episode of acute variceal bleeding.
REFERENCES
- http://www.webmd.com/digestive-disorders/digestive-diseases-portal
- Yoon Y, Yi H. Surveillance report no. 88: liver cirrhosis mortality in the United States, 1970-2007. National Institute on Alcohol Abuse and Alcoholism. Available at http://pubs.niaaa.nih.gov/publications/surveillance88/Cirr07.htm. Accessed: Jul 17 2012.
- Garcia-Tsao G, Sanyal AJ, Grace ND, Carey WD, and the Practice Guidelines Committee of the American Association for the Study of Liver Diseases, the Practice Parameters Committee of the American College of Gastroenterology. Prevention and management of gastroesophageal varices and variceal hemorrhage in cirrhosis. Am J Gastroenterol. 2007 Sep. 102(9):2086-102.
- Suhail Ahmed Almani, A. Sattar Memon, Amir Iqbal Memon, M. Iqbal Shah, M. Qasim Rahpoto, Rahim Solangi, Cirrhosis of liver: Etiological factors, complications and prognosis, JLUMHS MAY – AUGUST 2008.
- https://my.clevelandclinic.org/health/diseases/4912-portal-hypertension/management-and-treatment
