EPIDEMIOLOGY
Cancer is the second leading cause of death globally, and is responsible for an estimated 9.6 million deaths in 2018. Globally, about 1 in 6 deaths is due to cancer. Tobacco use is the most important risk factor for cancer and is responsible for approximately 22% of cancer deaths.(1)
In 2018, according to the GLOBOCAN estimates, there were 2,093,876 (11.6%) new cases of lung cancer identified worldwide. Lung cancer is the most commonly diagnosed cancer (11.6% of the total cases) and the leading cause of cancer death (18.4% of the total cancer deaths). In 2018, there were an estimated 1,761,007 deaths from lung cancer occurred worldwide (18.4% of the total number of cancer deaths).(2)
According to GLOBOCAN 2018, Pakistan has 9,771 (6.58%) new cases of lung cancer which makes it 3rd most common cancer in Pakistan. An estimated 9,260 (9.07%) deaths occurred in Pakistan due to lung cancer.(2)
PATHOPHYSIOLOGY
The pathogenesis of lung cancer is like other cancers, beginning with carcinogen-induced initiation events, followed by a long period of promotion and progression in a multistep process. Cigarette smoke both initiates and promotes carcinogenesis. The initiation event happens early on, as evidenced by similar genetic mutations between current and former smokers (e.g. 3p deletion, p53 mutations). Smoking thus causes a “field effect” on the lung epithelium, providing a large population of initiated cells and increasing the chance of transformation. Continued smoke exposure allows additional mutations to accumulate due to promotion by chronic irritation and promoters in cigarette smoke (e.g. nicotine, phenol, formaldehyde). The time delay between smoking onset and cancer onset is typically long, requiring 20-25 years for cancer formation. Cancer risk decreases after smoking cessation, but existing initiated cells may progress if another carcinogen carries on the process.(3)
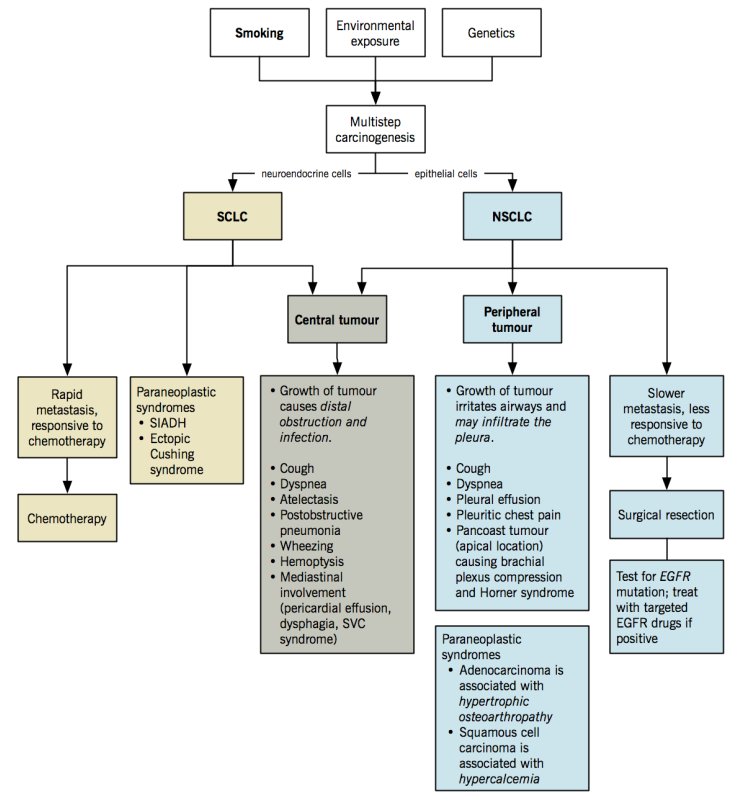
Small cell lung cancer (SCLC) and Non-small-cell lung cancer (NSCLC) are treated differently because they (i) originate from different cells, (ii) undergo different pathogenesis processes, and (iii) accumulate different genetic mutations. SCLC often harbors mutations in MYC, BCL2, c-KIT, p53, and RB, while NSCLC often has mutations in EGFR, KRAS, CD44, and p16. These are all either tumor suppressor genes or oncogenes.(4) Lung cancer pathophysiology overview is given in below figure.
TRANSMISSION(5)
A healthy person cannot “catch” cancer from someone who has it. There is no evidence that close contact or things like sex, kissing, touching, sharing meals, or breathing the same air can spread cancer from one person to another.
Cancer cells from one person are generally unable to live in the body of another healthy person. A healthy person’s immune system recognizes foreign cells and destroys them, including cancer cells from another person.
Cancer transfer during organ transplant
There have been some cases in which organ transplants from people with cancer have been able to cause cancer in the person who got the organ. But there’s a major factor that makes this possible – people who get organ transplants take medicines that weaken their immune systems. This must be done so their immune system won’t attack and destroy the transplanted organ. This seems to be the main reason that cancer in a transplanted organ can, in rare cases, give cancer to the person who gets the organ. Organ donors are carefully screened to reduce this risk.
Cancer risk after transplant already high
Still, recent studies have shown that cancer is more common in people who get solid-organ transplants than in people who don’t – even when the donor doesn’t have cancer. This also appears to be due to the drugs that are given to reduce the risk of transplant rejection. Research has shown that the longer and more intensely the immune system is suppressed after transplant, the higher the risk of cancer. The drugs that allow the body to accept the organ also make the immune system less able to recognize and attack pre-cancer cells and the viruses that can cause cancer.
Cancer transfer during pregnancy
Even if a woman has cancer during pregnancy, the cancer rarely affects the fetus directly. Some cancers can spread from the mother to the placenta but most cancers cannot affect the fetus itself. In a few very rare cases, melanoma has been found to spread to the placenta and the fetus.
NATURAL HISTORY(6)
There are two main ways to assess the natural history. The most obvious is to follow the outcomes of patients who were not treated with any therapeutic intervention (other than basic supportive care). Direct measurement of the natural history is simple but may be difficult to generalize. Those patients who choose or are chosen not to receive any active treatment may be quite different from those receiving treatments, because of comorbidities, psychologic or social issues, all of which have been shown to affect survival. The differences in the characteristics of treated and untreated patients are perhaps most marked in patients with early stage lung cancer, in whom definition of the natural history is most important.
Another way to estimate survival without treatment is based on observation of the tumor over a period of time, after which an intervention is (usually) undertaken. Estimation of the natural history from a period of observation is probably much more representative of the broad patient population with lung cancer. A period of observation may be more likely to have occurred in patients with slow growing tumors, although it is likely that this selection bias is relatively low. This suppositive is based on the high frequency of missed lesions seen retrospectively on chest radiographs and the frequency of an inherent period of observation of CT-detected lesions (e.g., interval between screening CT and diagnostic CT). However, there is uncertainty about how well the behavior during the period of observation can be extrapolated throughout the life of the tumor.
A systematic review of the data shows that untreated lung cancer is almost uniformly rapidly fatal, even if it is stage I. Analysis of data regarding tumor volume doubling times shows that conventionally detected lung cancers have short mean doubling times, and only a small proportion with very long doubling times. Lung cancers found during the course of a CT screening program have markedly longer mean doubling times and a substantially greater proportion with very long doubling times (>400 days). Models of tumor growth, however, are not understood well enough to use the observed doubling time to predict length of survival without treatment.
SIGN AND SYMPTOMS(7)
The most common symptoms of lung cancer are:
- A cough that does not go away or gets worse
- Coughing up blood or rust-colored sputum (spit or phlegm)
- Chest pain that is often worse with deep breathing, coughing, or laughing
- Hoarseness
- Weight loss and loss of appetite
- Shortness of breath
- Feeling tired or weak
- Infections such as bronchitis and pneumonia that don’t go away or keep coming back
- New onset of wheezing
If lung cancer spreads to distant organs, it may cause:
- Bone pain (like pain in the back or hips)
- Nervous system changes (such as headache, weakness or numbness of an arm or leg, dizziness, balance problems, or seizures), from cancer spread to the brain or spinal cord
- Yellowing of the skin and eyes (jaundice), from cancer spread to the liver
Lumps near the surface of the body, due to cancer spreading to the skin or to lymph nodes (collections of immune system cells), such as those in the neck or above the collarbone
RATIONALE FOR SCREENING(8)
As lung cancer predominantly affects smokers and individuals exposed to other carcinogens, screening programs need not include the whole population but only these risk groups. Every screening program will tend to better identify the more indolent tumors that grow slowly enough to be detected by screening before symptoms develop, whereas aggressive fast-growing tumors may present as interval cancers despite screening (length-time bias). Some malignant tumors detected with screening may never cause the person’s death due to competing causes for death, particularly in heavy smokers, such as cardiovascular disease or other cancers (over diagnosis bias). If a cancer is still lethal despite detection through screening, the affected individual may live longer with the diagnosis of cancer but no longer altogether (lead-time bias). It is likely that this will have a negative effect on that individual’s quality of life. Participation in screening programs may have beneficial as well as adverse effects on smoking habits; in the worst case it may encourage people to continue smoking. Trials assessing chest radiography or sputum microscopy have not demonstrated a reduction in lung cancer mortality through screening, probably because the tests were not sensitive enough, computed tomography promises better sensitivity. Other modern tests such as fibre optic bronchoscopy, analysis of molecular markers or genetic testing in serum, sputum or exhaled air are not yet ready for clinical practice.
DIAGNOSTIC TESTS (9)
The following tests are commonly used to rule out or diagnose lung cancer. Many of the same tests used to diagnose cancer are used to find out the stage.
Health history and physical exam
Ask following questions from patient:
- symptoms that suggest lung cancer
- smoking or breathing in second-hand smoke
- being around radon gas
- being around asbestos at work
- lung cancer or lung diseases
- radiation therapy to the chest area
Identify family history of:
- lung cancer
- other cancers
A physical examination should include:
- Examination of lungs and heart using a stethoscope
- Examine neck and area above the collarbone to look for swelling or lymph nodes that are larger than normal
- Examine abdomen for a liver that is larger than normal
- Blood pressure and pulse
Complete blood count (CBC)
A CBC is done to get some basic information about overall health before any treatments start.
Blood chemistry tests
- Alkaline phosphatase (ALP), calcium or phosphorus levels that are higher than normal may mean that cancer has spread to the bones.
- Liver function tests look at the levels of lactate dehydrogenase (LDH), alanine aminotransferase (ALT), aspartate transaminase (AST) and bilirubin. Higher levels may mean that cancer has spread to the liver.
X-ray
A chest x-ray is often the first imaging test done to look for problems with the lungs. It may show any spots, tumors or changes in the lungs.
Computed Tomography (CT) scan
A CT scan is used to:
- show the location, size and shape of a lung tumor
- find any lymph nodes in the chest that are larger than normal
- look for any spread of the tumor to other parts of the body
- guide a biopsy
Positron Emission Tomography (PET) scan
A PET scan is used to find out how far the lung cancer has spread as it looks at the whole body during the scan. It can find tumors over 8 mm in size. It is more accurate than CT scan for finding spread to the lymph nodes in the middle of the chest (mediastinum) and other areas of the body. PET scans are not used to look at the brain, because the brain has a high level of metabolic activity.
Magnetic resonance imaging (MRI)
An MRI is used to look at the brain to see if cancer has spread there. It may also be used to look at the heart before surgery to find out if the cancer has invaded the heart or the large blood vessels and nerves at the tip of the lung.
Ultrasound
An ultrasound uses high-frequency sound waves to make images of structures in the body. It is used to look for a buildup of fluid around the lungs. An ultrasound is also used to guide a biopsy during endoscopic procedures.
Biopsy
Getting enough tissue during a biopsy is important so that immunohistochemistry and molecular testing can be done. CT scans or ultrasounds are often used to guide the biopsy for lung cancer.
- Fine needle aspiration (FNA) uses a very thin needle and syringe to remove a sample of cells, tissue or fluid from an abnormal area or lump in the body. It can be used to diagnose lung cancer. An FNA is used during an endoscopy to sample the lymph nodes in between the lungs. An FNA can also be used to take samples from a possible tumor that is found in the outer part of the lungs. The needle is inserted through the skin of the chest and is guided to the area during a CT scan so that tissue can be removed.
- Core biopsy is like an FNA, except a larger needle or probe is used to remove tissue. Core biopsies can get larger amounts of tissue than an FNA, which helps with diagnosis and identifying the type of lung cancer.
- Thoracentesis is a procedure that uses a needle to remove fluid from around the lungs. The fluid is examined to see if it has any cancer cells in it.
- Surgical biopsy removes a piece of lung tissue so it can be examined. It is done through a cut (incision) made between the ribs.
Endoscopy
An endoscopy is done to remove tissue samples and to see how far lung cancer has spread. It allows looking inside the body using a flexible or rigid tube with a light and lens on the end. This tool is called an endoscope.
- Bronchoscopy is used to look inside the large airways of the lungs (the trachea and bronchi) for a tumor or a blockage. Special bronchoscopes with an ultrasound sensor (endobronchial ultrasound or EBUS) allow biopsy of lymph nodes close to the trachea and bronchi for diagnosis or to find out if cancer has spread to the lymph nodes. Lymph nodes can also be sampled by ultrasound scopes inserted into the esophagus (EUS).
- Mediastinoscopy is used to look at the area between the lungs called the mediastinum. Lymph nodes and other tissue samples near the trachea may be removed during a mediastinoscopy. Mediastinoscopy is only used if an EBUS is negative but the lymph nodes are still suspicious for cancer.
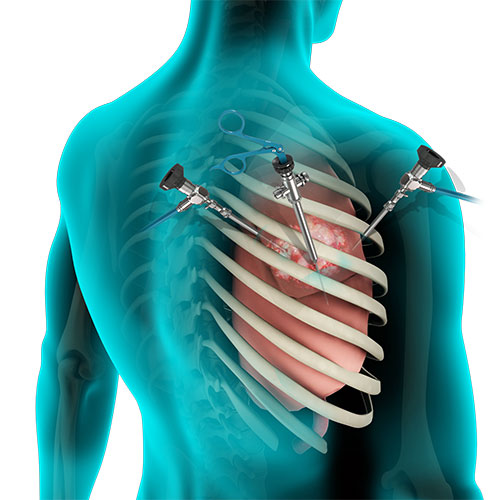
- Thoracoscopy is used to look inside the chest cavity, including the chest wall, the lining of the lungs, and the lymph nodes in the chest. It may be done if other tests can’t get enough tissue for a diagnosis.
Sputum tests
Sputum may be examined to see if it contains cancer cells. Several sputum samples are collected (usually in the early morning). If people have trouble coughing up sputum, they may be given a mist to inhale to help them cough.
Tumors in the large bronchi of the lung, squamous cell tumors and large tumors may shed cancer cells into the sputum.
Immunohistochemistry
Immunohistochemistry tests look for certain proteins (called antigens) that are found on the surface of cells. These tests can help identify the type and subtype of lung cancer.
Anaplastic lymphoma kinase (ALK) is a gene that controls the growth of cells. Immunohistochemistry staining can identify mutations in the ALK gene. ALK mutations in non–small cell lung cancer are more common in non-smokers or light smokers. Another immunohistological test may be done to look for changes in the immune cells such as PD-L1.
The results of immunohistochemistry tests help to decide which treatment is the best option, based on the cancer that is identified.
Molecular tissue tests
Molecular tissue tests look for certain changes (mutations) in the genes of lung cancer cells. These changes affect the type of treatment given because some chemotherapy drugs may be more useful against cancer cells with these changes.
Molecular tissue tests for lung cancer look for certain gene changes.
- Epidermal growth factor receptor (EGFR) is a protein found on the surface of cells that helps cells grow. Changes in the EGFR gene can cause a higher than normal amount of EGFR in some types of lung cancer. These changes are more common in non-smokers, women and people with Asian ancestry. This is the most common molecular tissue test used for lung cancer.
- BRAF is a protein that sends signals in cells and helps with cell growth. Changes in the BRAF gene, called BRAF-V600E, can be found in higher amounts in some types of lung cancer.
- ROS1 is another protein that sends signals in cells and helps with cell growth. Changes in the ROS1 gene can be found in higher than normal amounts in some types of lung cancer. These changes are more often seen in younger people or non-smokers and light smokers.
Bone scan
A bone scan uses bone-seeking radioactive materials and a computer to create a picture of the bones. It is done in people who have bone pain or if blood chemistry tests suggest that cancer has spread to the bones.
Pulmonary function tests
Pulmonary function tests check how well the lungs are working. They measure how much air the lungs can hold and how well the person can let air out of the lungs. These tests are important if doctors are considering surgery as a treatment option for lung cancer. They help make sure that the person will have enough lung capacity after a lung or part of a lung is removed.
An arterial blood test may be done with pulmonary function tests. A small needle is used to remove blood from a small artery, usually on the back of the hand or on the wrist. The blood is tested for the levels of oxygen and carbon dioxide.
PATIENT SELECTION FOR TREATMENT(10)
Before treatment, a biopsy is usually performed to determine whether a patient has cancer, and if so, what type.
Tests are recommended to determine the stage of the tumor. These tests usually include blood tests and imaging. The imaging usually includes computed tomography (CT) scanning of the chest, and may include a bone scan or a PET/CT scan. The treatment options and expected results of treatment depend on the stage of the tumor.
TREATMENT OPTIONS
Treatment depends on the type of lung cancer. The treatment for non small cell lung cancer is different from the treatment for small cell lung cancer.
Small Cell Lung Cancer
Small Cell Lung Cancer is mostly treated with chemotherapy. Surgery is only suitable if there is no sign that the cancer has spread to the lymph glands in the centre of the chest (the mediastinal lymph glands). This is rare with small cell lung cancer. It has usually spread at the time of diagnosis. So chemotherapy is usually the main treatment. Radiotherapy can be done to treat this type of lung cancer.(11)
Treatments for small cell lung cancer may include a combination of different types of treatments, such as:
- Chemotherapy
- Radiation therapy and/or surgery. (12,13)
Chemotherapy: A chemotherapy regimen usually consists of a specific number of cycles given over a set period of time. A patient may receive one drug at a time or combinations of different drugs at the same time.
Chemotherapy is the primary treatment for small cell lung cancer because it spreads quickly. The most commonly used chemotherapy regimen is
- Etoposide
- Irinotecan plus a platinum-based drug such as cisplatin or carboplatin
For patients with limited stage small cell lung cancer, chemotherapy plus radiation therapy to the chest is given daily over several weeks. Patients with extensive stage cancer initially receive chemotherapy for 3 to 4 months.
Radiation therapy: Radiation therapy is the use of high energy x-rays or other particles to destroy cancer cells. The most common type of radiation treatment is called external-beam radiation therapy, which is radiation given from a machine outside the body. A radiation therapy regimen (schedule) usually consists of a specific number of treatments given over a set period of time. This can vary from just a few days of treatment to several weeks.
For patients with limited stage small cell lung cancer, radiation therapy is combined with chemotherapy. Radiation therapy is best when given during the first or second month of chemotherapy.
In patients whose cancer has shrunk after chemotherapy, radiation therapy to the head lessens the risk that the cancer will spread to the brain. This is called prophylactic cranial irradiation (PCI), and it has been shown to lengthen the lives of these patients.(12,13)
If the radiation therapy irritates or inflames the lung, patients may develop a cough, fever, or shortness of breath months and sometimes years after the radiation therapy ends. About 15% of patients develop this condition, called radiation pneumonitis. If it is mild, radiation pneumonitis does not need treatment and goes away on its own. If it is severe, a patient may need treatment for radiation pneumonitis with steroid medications, such as prednisone. Radiation therapy may also cause permanent scarring of the lung tissue near where the original tumor was located. Typically, the scarring does not cause symptoms. However, severe scarring can cause a permanent cough and shortness of breath. For this reason, radiation oncologists carefully plan the treatments using CT scans of the chest to lessen the amount of healthy lung tissue exposed to radiation.
Surgery: Surgery is rarely used for patients with small cell lung cancer and is only considered for patients with very early-stage disease, such as cancer in a small lung nodule. In those situations, chemotherapy, with or without radiation therapy, is given after surgery.
Non Small Cell Lung Cancer(14)
Non Small Cell Lung Cancer can be treated with surgery, chemotherapy, radiotherapy or a combination of these, depending on the stage when the cancer is diagnosed. Some people with advanced lung cancer may have biological therapy.
Targeted therapy:Targeted therapy is a treatment that targets the cancer’s specific genes, proteins, or the tissue environment that contributes to cancer growth and survival. This type of treatment blocks the growth and spread of cancer cells while limiting damage to healthy cells.
- Anti-angiogenesis therapy: Anti-angiogenesis therapy is focused on stopping angiogenesis, which is the process of making new blood vessels. Because a tumor needs the nutrients delivered by blood vessels to grow and spread, the goal of anti-angiogenesis therapies is to “starve” the tumor. Bevacizumab is an anti-angiogenic drug given along with chemotherapy for lung cancer. The risk of serious bleeding for patients taking bevacizumab is about 2%. However, it is more common for patients with squamous cell carcinoma, so bevacizumab is usually not recommended for patients with this type of NSCLC.
Drugs that work on specific mutations in cancer cells. Researchers have found that drugs that block the epidermal growth factor receptor (EGFR) may be effective for stopping or slowing the growth of lung cancer.
- Erlotinib is a drug that blocks the EGFR. This drug has been shown to work better than chemotherapy if the lung cancer has a mutation in the EGFR gene. It is approved by the U.S. Food and Drug Administration (FDA) for patients with locally advanced and metastatic NSCLC and as a maintenance therapy for patients with NSCLC that has not grown or spread after at least four cycles of chemotherapy.
- Gefitinib is another drug that blocks the EGFR.
- Afatinib was approved by the FDA in 2013 as an initial treatment for NSCLC. It is a type of drug called a tyrosine kinase inhibitor (TKI) that works by stopping uncontrolled cell growth caused by a mutation in the EGFR gene.
- Crizotinib is another type of targeted therapy approved by the FDA for advanced NSCLC that has a mutation in the ALK gene.
- Ceritinib is an additional targeted therapy for NSCLC with an ALK gene mutation. It is approved by the FDA for patients when the cancer worsens while they are receiving crizotinib or if they cannot take crizotinib.
- Ramucirumab is another type of anti-angiogenic drug approved for NSCLC along with the drug docetaxel.
Immunotherapy: Immunotherapy, also called biologic therapy, is designed to boost the body’s natural defenses to fight the cancer. It uses materials made either by the body or in a laboratory to improve, target, or restore immune system function. For example, the PD-1 pathway may be critical in the immune system’s ability to control cancer growth. Blocking this pathway with PD-1 and PD-L1 antibodies has stopped or slowed the growth of NSCLC for some patients.
- Nivolumab is the first of these types of drugs to be approved for NSCLC.
- Pembrolizumab is another type of these drugs recently approved for NSCLC that has spread after patients have received other treatments.
Palliative care: Palliative care will also be important to help relieve symptoms and side effects. Radiation therapy or surgery may also be used to treat metastases that are causing pain or other symptoms. Bone metastases that weaken major bones can be treated with surgery, and the bones can be reinforced using metal implants. (15)
GOALS OF THERAPY
The overall goal of cancer treatment is to significantly decrease the number of deaths, relieve symptoms, prolong life and maintain quality of life.(16)
GUIDELINES
To view, “NCCN Guideline on Non-small Cell Lung Cancer 2016”, please click on below link:
http://www.hts.org.gr/assets/files/omades_ergasias/cancer/NCCN%20guidelines%20NSCLC%202016.pdf
To view, “NCCN Guideline on Small Cell Lung Cancer 2016”, please click on below link:
https://www2.tri-kobe.org/nccn/guideline/lung/english/small.pdf
To view, “SIGN Guidelines for Lung Cancer”, please click on below link:
https://www.sign.ac.uk/sign-137-management-of-lung-cancer.html
To view, “ESMO Consensus Guidelines: Locally-advanced stage III non-small-cell lung cancer (NSCLC)”, please click on below link:
http://www.esmo.org/Guidelines/Lung-and-Chest-Tumours/Consensus-Guidelines-Locally-advanced-stage-III-non-small-cell-lung-cancer-NSCLC
To view, “Metastatic Non-Small-Cell Lung Cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up”, please click on below link:
http://www.esmo.org/Guidelines/Lung-and-Chest-Tumours/Metastatic-Non-Small-Cell-Lung-Cancer
To view, “ESMO Consensus Guidelines: Non-small-cell lung cancer first-line/second and further lines in advanced disease”, please click on below link:
http://www.esmo.org/Guidelines/Lung-and-Chest-Tumours/Consensus-Guidelines-Non-small-cell-lung-cancer-first-line-second-and-further-lines-in-advanced-disease
To view, “Small-Cell Lung Cancer: ESMO Clinical Practice Guidelines”, please click on below link:
http://www.esmo.org/Guidelines/Lung-and-Chest-Tumours/Small-Cell-Lung-Cancer
CONSULTATION AND LONG TERM MONITORING
Small Cell Lung Cancer (SCLC)
Patients with small cell lung cancer (SCLC) require close monitoring for adverse effects and response to therapy. Blood work, including a complete blood count (CBC) with differential, is needed before each cycle of chemotherapy to ensure marrow recovery before the next dose of chemotherapy is administered. Renal function should be monitored because of nephrotoxicity from cisplatin.
Serum lactate dehydrogenase (LDH), if elevated before the start of therapy, is a good marker for response and should be monitored. In addition, computed tomography (CT) scans should be obtained after 2 cycles of therapy to assess response before chemotherapy is continued. In general, patients who are asymptomatic require follow-up only as clinically needed.
Patients who smoke cigarettes should be encouraged to quit. A meta-analysis by Parsons et al suggested that smoking cessation after diagnosis of early stage lung cancer may improve prognosis, probably by reducing cancer progression. Evaluation of data from 9 studies showed that the estimated 5-year survival rate in limited-stage SCLC was 63% in patients who quit smoking, versus 29% in those who continued to smoke.(17)
Non Small Cell Lung Cancer (SCLC)
Recommendations from the National Comprehensive Cancer Network (NCCN) regarding cancer surveillance in survivors of non – small cell lung cancer (NSCLC) include the following :
- History and physical examination and chest computed tomography (CT) scan with or without contrast every 6-12 months for 2 years, then an H&P and noncontrast chest CT scan annually.
- Assessment of smoking status at each visit, with counseling and referral for smoking cessation as needed.
Other NCCN recommendations for long-term follow-up care include the following:
- Immunization: Annual influenza vaccination, pneumococcal vaccination with revaccination as appropriate, herpes zoster vaccination
- Counseling regarding health promotion and wellness (e.g. regular physical activity, healthy diet)
- Routine health monitoring. (17)
