EPIDEMIOLOGY
Bladder cancer is the ninth most common cancer in the world, with 430,000 new cases diagnosed in 2012.(1) In the United States, approximately 81,000 new cases and 17,000 deaths occur each year due to bladder cancer.(2) In Europe, there were an estimated 118,000 cases and 52,000 deaths in 2012.(3)
In Pakistan, urinary bladder cancer is one of the top ten malignancies in men and the most common urological malignancy in both sexes.(4) According to the report of Shaukat Khanum Memorial Trust carried out during Jan 2016 to Dec 2016 which included patients registered at the centers, bladder cancer is found to be the 8th common cancer in males accounting for 5.10%.(5)
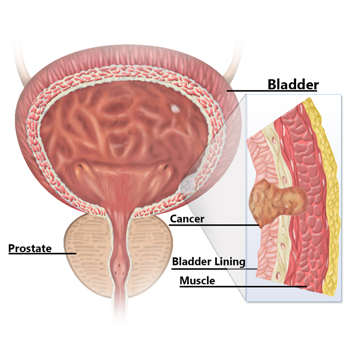
PATHOPHYSIOLOGY(6)
Bladder cancer is often described as a polyclonal field change defect with frequent recurrences due to a heightened potential for malignant transformation. However, bladder cancer has also been described as resulting from implantation of malignant cells that have migrated from a previously affected site. The latter occurs less often and may account for only a small percentage of cases.
The WHO classifies bladder cancers as low grade (grades 1 and 2) or high grade (grade 3). Tumors are also classified by growth patterns: papillary (70%), sessile or mixed (20%), and nodular (10%).
Transitional cell carcinoma
Transitional cell carcinoma (TCC) arises from stem cells that are adjacent to the basement membrane of the epithelial surface. Depending on the genetic alterations that occur, these cells may follow different pathways in the expression of their phenotype.
The most common molecular biologic pathway for TCCs involves the development of a papillary tumor that projects into the bladder lumen and, if untreated, eventually penetrates the basement membrane, invades the lamina propria, and then continues into the bladder muscle, where it can metastasize. Nearly 90% of transitional cell bladder tumors exhibit this type of behavior
This progression occurs with high-grade cancers only. Low-grade cancers rarely, if ever, progress and are thought to have a distinct molecular pathway, different from the high-grade cancers and CIS.
The remaining 10% of TCCs follow a different molecular pathway and are called CIS. This is a flat, noninvasive, high-grade urothelial carcinoma tumor that spreads along the surface of the bladder and, over time, may progress to an invasive form of cancer that behaves the same as invasive TCC.
Many urothelial tumors are primarily composed of TCC but contain small areas of squamous differentiation, squamous cell carcinoma (SCC), or adenocarcinoma.
Squamous Cell Carcinoma
SCC of the urinary bladder is a malignant neoplasm that is derived from bladder urothelium and has a pure squamous phenotype. SCC of the bladder is essentially similar to squamous cell tumors arising in other organs. Because many urothelial carcinomas contain a minor squamous cell component, a diagnosis of SCC of the bladder should be rendered only when the tumor is solely composed of squamous cell components, with no conventional urothelial carcinoma component.
Reportedly, SCC has less of a tendency for nodal and vascular distant metastases than does urothelial carcinoma.
Genetic factors in pathogenesis
Divergent, yet interconnected and overlapping, molecular pathways are likely responsible for the development of noninvasive and invasive bladder tumors. Somatic mutations in fibroblast growth receptor3 (FGFR-3) and tumor protein p53 (TP53) in tumor cells appear to be important early molecular events in the noninvasive and invasive pathways, respectively.
FGFR-3, Ras, and PIK3CA mutations occur with high frequency in noninvasive tumors, leading to upregulation of Akt and mitogen-activated protein kinase (MAPK). Loss of heterozygosity (LOH) on chromosome 9 is among the most frequent genetic alterations in bladder tumors and is considered an early event.
Large numbers of genomic changes have been detected using karyotyping and comparative genomic hybridization (CGH) analysis in urothelial carcinoma. Numerically common are losses of 2q, 5q, 8p, 9p, 10q, 18q, and Y. Gains of 1q, 5p, 8q, and 17q are frequently present, and high-level amplifications can be found; however, the target genes in the regions of amplifications have not been conclusively identified.
Alterations in the TP53 gene are noted in approximately 60% of invasive bladder cancers. Progression-free survival is significantly shorter in patients with TP53 mutations and is an independent predictor of death among patients with muscle-invasive bladder cancer.
Additionally, alterations in retinoblastoma (Rb), PTEN, and p16 are common in high-grade invasive cancers. Overexpression of JUN, MAP2K6, STAT3, and ICAM1 and molecules associated with survival (Bcl-2, caspase-3, p53, survivin), as well as insensitivity to antigrowth signals (p53, p21, p16, pRB), has been demonstrated.
In advanced disease, multiple mechanisms may lead to tumor progression. These include those that promote proliferation, survival, invasion, and metastasis, as well as those that involve deficiencies in DNA damage repair and the finding of stemlike cells.
In addition to tumor cell alterations, the microenvironment may promote tumor growth by paracrine influences, including vascular endothelial growth factor (VEGF) production and aberrant E-cadherin expression. Finally, a growing body of research over the last decade indicates that epigenetic alterations may silence tumor suppressor genes and that they represent important events in tumor progression.
Natural history(7)
The natural history of bladder cancer can be correlated with several prognostic factors. These include histological grade, the depth of penetration into the bladder wall (stage), the appearance of vascular/lymphatic invasion, and the presence of carcinoma in situ (CIS). Although these indicators of prognosis are widely recognized, the biologic basis for the subsets of disease within each of these categories is incompletely understood.
Some tumors appear to have favorable histology but progress and express aggressive activity despite theoretically curative treatments, whereas other tumors appear to have unfavorable histology and yet are less aggressive or at least more amenable to cure. Although clinically useful, histological assessment is not a sufficiently sensitive discriminant in determining the specific biologic potential of a particular cancer. Therefore, an assessment of the genetics and molecular biology of a tumor and of the entire process of carcinogenesis is warranted.
SIGN AND SYMPTOMS(6)
Approximately 80-90% of patients with bladder cancer present with painless gross hematuria. All patients with this classic presentation should be considered to have bladder cancer until proof to the contrary is found.
Irritative bladder symptoms such as dysuria, urgency, or frequency of urination occur in 20-30% of patients with bladder cancer. Although irritative symptoms may be related to more advanced muscle-invasive disease, carcinoma in situ (CIS) is the more likely cause. Therefore, patients presenting with unexplained or refractory irritative symptoms should be considered for cystoscopy and urine cytology. The threshold for doing so should be especially low in persons who smoke or have other risk factors.
Patients with advanced disease can present with pelvic or bony pain, lower-extremity edema from iliac vessel compression, or flank pain from ureteral obstruction.
Physical Examination
Non ̶ muscle-invasive bladder cancer is typically not found during a physical examination. In rare cases, a mass is palpable during abdominal, pelvic, rectal, or bimanual examination. A bimanual examination may be considered part of the staging of such lesions. In women, a bimanual pelvic examination is done; in men, a bimanual examination is performed with one hand per rectum and the other on the lower abdominal wall.
Attention to the anterior vaginal wall in women and the prostate in men may reveal findings that suggest local extension of bladder cancer. Assessment of fixation of the bladder to the surrounding pelvic sidewall is also important when planning definitive management for locally advanced tumors that may not be surgically resectable.
RATIONALE FOR SCREENING
In 2011, the US Preventive Services Task Force (USPSTF) concluded that the evidence was insufficient to determine the balance of benefits and harms of screening for bladder cancer in asymptomatic adults. Although adults with mild lower urinary tract symptoms (e.g., urinary frequency, hesitancy, urgency, dysuria, nocturia) are not strictly asymptomatic, these symptoms are common and are not believed to be associated with an increased risk of bladder cancer. The USPSTF considered it reasonable to include these persons in the population under consideration for screening. Adults with gross hematuria or acute changes in lower urinary tract symptoms were not included in this population.(8)
No major organization recommends screening for bladder cancer in asymptomatic adults. In 2011, the American Academy of Family Physicians endorsed the USPSTF recommendation.(9) The American Cancer Society states that prompt attention to bladder symptoms is the best approach for finding bladder cancer in its earliest, most treatable stages in persons with no known risk factors.(10)
Diagnostic tests(6)
Urine studies include the following:
- Urinalysis with microscopy
- Urine culture to rule out infection, if suspected
- Voided urinary cytology
- Urinary tumor marker testing
Urinalysis is performed to detect hematuria or infection. Microscopic hematuria from bladder cancer may be intermittent; therefore, a repeat negative result on urinalysis does not exclude the diagnosis.
Cytology
Urinary cytology is extremely valuable and is often the test used for diagnosis; suggestive urine cytology findings should encourage the urologist to perform a cystoscopy and possibly bladder biopsy. All patients with gross hematuria and many with significant microscopic hematuria should undergo a cystoscopy and urinary cytology (preferably barbotage urine for cytology).
Urinary cytology is most helpful in diagnosing high-grade tumors and carcinoma in situ (CIS). Low-grade, noninvasive tumors may be missed by routine cytologic analysis.
Endoscopic biopsies are used to establish the diagnosis and determine the extent of the cancer. However, a study by Cha et. al. found that immunocytology outperforms urine cytology and increases the accuracy of predictive models by a statistically and clinically significant margin for patients with painless hematuria.(11)
Strittmatter et. al. found that the quality of urinary cytology is impacted by the individual learning curve. Specificity of cytology and sensitivity for low-grade tumors significantly changed when performed by a local cytologist at the beginning of the learning period. This suggests that in the diagnosis of bladder cancer, the cytologist’s level of experience has an important impact on the clinical value of urinary cytology.(12)
Findings: Because cytology is the most reliable urine test for detecting bladder cancer, a positive cytology finding should be treated as indicating cancer until proven otherwise. If cystoscopy findings are negative in the setting of positive cytology findings, further evaluation of the urinary tract is required. The upper urinary tract should be evaluated with contrast imaging. Cystoscopy with bilateral retrograde pyelography and bilateral ureteral washings should be performed.
Most patients with CIS have coexisting papillary cancer. In general, the papillary tumor is diagnosed first, and CIS is discovered during the evaluation and treatment of the papillary tumor. Only 10% of patients with bladder cancer have a pure CIS. The combination of CIS and papillary transitional cell carcinoma (TCC) is associated with a higher risk of recurrence and progression.
In cases of pure CIS, urinary cytology may lead to the diagnosis. CIS exfoliates cells that have an unusual appearance and are easy to identify via cytologic examination, prompting further evaluation. Unfortunately, even findings from urine cytology may be normal in some patients; in these cases the diagnosis is made only when the urologist maintains a high level of suspicion for CIS and obtains random bladder biopsy specimens from patients with worrisome symptoms. However, if the urinary cytology is performed properly, this should happen rarely.
Cystoscopy
Cystoscopy is the criterion standard for detecting bladder cancer, but it is invasive and relatively expensive. Moreover, visibility can be reduced by bleeding, and flat urothelial lesions such as CIS may be difficult to distinguish from normal bladder tissue. Use of adjunctive endoscopic techniques, such as blue light cystoscopy with 5-aminolevulinic acid, may improve the accuracy of cystoscopy. Cytologic analysis of voided urine is frequently used as an adjunctive test to aid in identifying occult cancers.
Virtual cystoscopy can help detect many bladder tumors, but it is more expensive than cystoscopy and has lower sensitivity and specificity. Therefore, it does not play a role in surveillance at this time.
Imaging studies
Imaging studies of the upper urinary tract are an integral part of the hematuria workup. Computed tomography (CT) scans of the abdomen and pelvis with contrast are recommended. Two commonly used alternative techniques are magnetic resonance imaging (MRI) and renal ultrasonography. Few US centers still perform intravenous pyelography (IVP) for upper tract imaging.
The bladder urothelium is not well visualized with routine imaging studies, including CT scanning and MRI. Small tumors are easily missed on images produced by these modalities. Irregular areas on images, which may appear to represent mucosal abnormalities, are often artifacts of incomplete bladder filling; delayed images following contrast administration can better visualize actual filling defects. CIS is not visible on images from any current radiographic study.
Other tests
Markers: Newer molecular and genetic markers, including detection of mutations in genes such as RAS, FGFR3,PIK3CA, and TP53, and methylation pathways in urinary sediment, may help in the early detection and prediction of urothelial carcinoma. At this time, however, no urinary assay has been shown to effectively replace urine cytology and cystoscopy, with or without biopsy, for the diagnosis of bladder cancer. Nevertheless, marker assays may be useful adjuncts to urine cytology and cystoscopy.
Blood tests: No blood tests are specific for bladder cancer. In patients with CIS, however, a general evaluation is necessary prior to initiating therapy with intravesical bacillus Calmette-Guérin (BCG) vaccine.
THERAPY CONSIDERATION(6)
The treatment of non–muscle-invasive (Ta, T1, carcinoma in situ [CIS]) and muscle-invasive bladder cancer should be differentiated. Treatments within each category include surgical and medical approaches. European Association of Urology (EAU) and National Comprehensive Cancer Network (NCCN) guidelines for non–muscle-invasive cancer strongly recommend stratifying risk of recurrence and progression and using risk tables to determine appropriate treatment.(13,14)
The two principal treatment choices in muscle-invasive bladder cancer are radical cystectomy and transurethral resection of bladder tumor (TURBT) followed by concurrent radiation therapy and systemic chemotherapy (trimodality therapy). Each choice has its advocates.
TREATMENT OPTIONS
Immunotherapy and chemotherapy
Patients with low-grade, low-stage disease may receive expectant treatment or may benefit from a single instillation of intravesical chemotherapy. Both guidelines also recommend 1 immediate instillation of chemotherapy as the entire adjuvant treatment for patients at low risk of recurrence and progression.(13,14)
Bacillus Calmette-Guérin (BCG) immunotherapy or other intravesical chemotherapies may be used for patients with recurrent disease or those at intermediate risk, although they are not necessary for all high-risk patients. Patients with T1-high grade or CIS are advised to undergo intravesical BCG immunotherapy because of the substantial risk of disease recurrence and progression.
For patients with TaT1 tumors at intermediate risk of progression and intermediate or high risk of recurrence, EAU guidelines recommend 1 immediate instillation of chemotherapy followed by at least 1 year of intravesical BCG treatment or by further instillations of chemotherapy. Patients with Ta or T1 tumors and high risk of progression should receive 1 year of BCG treatment rather than further chemotherapy, as should patients with bladder CIS.
In May 2016, the FDA granted accelerated approval of atezolizumab, the first cancer immunotherapy that acts as an inhibitor of programmed cell death ligand 1 (PD-L1) for the treatment of urothelial carcinoma. Nivolumab, another PD-L1 inhibitor, also was approved by the FDA in February 2017.
Surgery and radiation therapy
Endoscopic treatment with transurethral resection of bladder tumor (TURBT) is the first-line treatment to diagnose, stage, and treat visible tumors. TURBT is not effective for CIS, because the disease is often so diffuse and difficult to visualize that complete surgical removal may not be feasible. It is critically important to surgically remove all non–muscle-invasive disease prior to beginning intravesical therapy. When a combination of papillary tumor and CIS is present, the papillary tumor is removed before treatment of the CIS is initiated.
The EAU guidelines recommend the use of fluorescence-guided resection, as it is more sensitive than conventional white-light cystoscopy for detection of tumors. The added detection rate with fluorescence-guided cystoscopy is 20% for all tumors and 23% for CIS. The FDA has approved the use of blue-light cystoscopy with 5-aminolevulinic acid (Cysview) in patients suspected or known to have non–muscle-invasive bladder cancer on the basis of prior cystoscopy.
As many as 20% of patients initially diagnosed with CIS may have unrecognized invasion beyond the lamina propria. Thus, they may not respond to intravesical therapy. These patients are candidates for radical cystectomy or radiation therapy and/or chemotherapy. Radiation therapy with or without chemotherapy is of limited benefit in patients with pure CIS but can be useful in some patients with muscle-invasive transitional cell carcinoma (TCC).
The criterion standard for the treatment of patients with stage T2-T4 disease is radical cystoprostatectomy for men and anterior pelvic exenteration for women. Additionally, all patients should undergo bilateral pelvic lymphadenectomy.
Level 1 evidence supports the use of preoperative (neoadjuvant) chemotherapy in patients with muscle-invasive bladder cancer. In addition, a series of studies have shown substantial benefit for adjuvant chemotherapy in these patients.
Lymph node dissection
Much controversy exists regarding the optimal extent of the lymph node dissection that should accompany cystectomy. It is clear that at minimum, a meticulous standard dissection should be performed.
While a number of retrospective studies demonstrate no difference in overall survival with standard versus extended lymph node dissection, a growing body of evidence suggests that more extended node dissection may improve survival in lymph node–positive and lymph node–negative disease.
Small cell carcinoma
The treatment of localized small cell carcinoma is neoadjuvant chemotherapy followed by radical cystectomy or external beam radiation therapy. Chemotherapy using a platinum-based protocol is applied to metastatic disease. In addition, adjuvant therapy may be used in cases of stage III and IV disease that were treated with radical cystectomy.
Adenocarcinoma
Adenocarcinomas respond poorly to radiation and chemotherapy. Radical cystectomy is the treatment of choice. Lymphomas may be effectively treated with chemotherapy or radiation.
Squamous cell carcinoma
For patients with squamous cell carcinoma (SCC) and those with squamous differentiation, a study by Ehdaie et al found no difference between the 2 groups regarding cancer-specific and overall survival following treatment with radical cystectomy and pelvic lymph node dissection.(15)
GOALS OF THERAPY
The main goals of a cancer treatment is to cure or considerably prolong the life of patients and to ensure the best possible quality of life to cancer survivors
GUIDELINES
To view, “Diagnosis and Treatment of Non-Muscle Invasive Bladder Cancer: American Urological Association / Society of Urological Oncology (AUA/SUO) guidelines”, please click on the link below.
https://insights.ovid.com/pubmed?pmid=27317986
To view, “Updated 2016 the European Association of Urology (EAU) Guidelines on Muscle-invasive and Metastatic Bladder Cancer”, please click on below link:
https://uroweb.org/…/EAU-Guidelines-Muscle-invasive-and-Metastatic-Bladder-Cancer
To view, “Bladder cancer: European Society of Medical Oncology (ESMO) Practice Guidelines for diagnosis, treatment and follow-up”, please click on below link:
https://academic.oup.com/annonc/article/25/suppl_3/iii40/1741392
To view, “National Comprehensive Cancer Network (NCCN) guidelines on Bladder cancer Version 1. 2014”, please click on below link:
http://www.cus.cz/wp-content/uploads/2012/10/NCCN-C67-2014.pdf
CONSULTATION AND LONG TERM MONITORING
For people treated for bladder cancer, follow-up care typically includes a general physical examination, cystoscopy (if the bladder has not been removed), urine cytology, x-rays, and routine blood tests to make sure the bladder is working well and to check for any signs that the cancer has come back.
For people with a urinary diversion, follow-up care may include checking for infection with urine tests, checking and fixing problems with controlling urination, checking for recurrent cancer in the upper urinary tract, and checking for changes in kidney function with blood tests and x-rays.
Watching for recurrence
One goal of follow-up care is to check for a recurrence. Cancer recurs because small areas of cancer cells may remain undetected in the body. Over time, these cells may increase in number until they show up on test results or cause signs or symptoms.
NCCN recommendations for follow-up after radical cystectomy
For follow-up after a radical cystectomy, NCCN recommendations are as follows:(14)
- Urine cytology, liver function tests, creatinine, and electrolytes every 3 to 6 mo for 2 y and then as clinically indicated
- Imaging of the chest, upper urinary tracts, abdomen, and pelvis every 3 to 6 mo for 2 y, based on risk of recurrence, and then as clinically indicated
- Consider urethral wash cytology every 6 to 12 mo, particularly if Tis was found within the bladder or prostatic urethra
- If a continent diversion was created, monitor for vitamin B12 deficiency annually
For follow-up after a segmental (partial) cystectomy or bladder preservation, the NCCN recommends the same follow-up as after radical cystectomy, plus cystoscopy and urine cytology with or without selected mapping biopsy every 3 to 6 mo for 2 y, then at increasing intervals as appropriate.
PRECAUTIONS
Advice following precautions to the patients:
- Quit Smoking: Smoking is thought to cause about half of all bladder cancers.
- Limit exposure to certain chemicals in the workplace: Workers in industries that use certain organic chemicals may have a higher risk of bladder cancer. Workplaces where these chemicals are commonly used include the rubber, leather, printing materials, textiles, and paint industries. Some chemicals found in certain hair dyes might also increase risk, so it’s important for hairdressers and barbers who are exposed to these products regularly to use them safely. Some research has suggested that people exposed to diesel fumes in the workplace might also have a higher risk of bladder cancer (as well as some other cancers), so limiting this exposure might be helpful.
- Drink plenty of liquids: There is some evidence that drinking a lot of fluids – mainly water – might lower a person’s risk of bladder cancer.
Eat lots of fruits and vegetables: Some studies have suggested that a diet high in fruits and vegetables might help protect against bladder cancer, but other studies have not found this. Still, eating a healthy diet has been shown to have many benefits, including lowering the risk of some other types of cancer.
REFERENCES
- Torre LA, Bray F, Siegel RL, et al. Global cancer statistics, 2012. CA Cancer J Clin 2015; 65:87.
- Siegel RL, Miller KD, Jemal A. Cancer statistics, 2018. CA Cancer J Clin 2018; 68:7.
- Marcos-Gragera R, Mallone S, Kiemeney LA, et al. Urinary tract cancer survival in Europe 1999-2007: Results of the population-based study EUROCARE-5. Eur J Cancer 2015.
- Rafique M, Javed AA. Role of itravenous urography and transabdominal ultrasonography in the diagnosis of bladder carcinoma. Int Braz J Urol 2004; 30: 185-91.
- Mahmood S, Faraz R et al. Annual Cancer Registry Report-2016, of the Shaukat Khanum Memorial Cancer Hospital & Research Center, Pakistan [Internet]. Available from: http://shaukatkhanum.org.pk/wp-content/uploads/2015/06/acrr-2016.pdf [Accessed on 2019 Jan 18)
- Gary David. Bladder Cancer. Medscape. New York. Available from: https://emedicine.medscape.com/article/438262-overview#a5 (Accessed on 2019 Jan 18)
- Richard Lee, Michael J. Droller. The Natural History of Bladder Cancer. Implications for Therapy. FEBRUARY 2000. Volume 27. Number 1.
- Moyer VA, U.S. Preventive Services Task Force. Screening for bladder cancer: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2011 Aug 16. 155 (4):246-51.
- Recommendations for Clinical Preventive Services: Bladder Cancer, Adults. Leawood, KS: American Academy of Family Physicians; 2011. American Academy of Family Physicians. Available at http://www.aafp.org/patient-care/clinical-recommendations/all/bladder-cancer.html. Accessed: May 11, 2017.
- Bladder Cancer. American Cancer Society. Available at https://www.cancer.org/cancer/bladder-cancer.html. May 23, 2016; Accessed: August 16, 2018.
- Cha EK, Tirsar LA, Schwentner C, Christos PJ, Mian C, Hennenlotter J, et al. Immunocytology is a strong predictor of bladder cancer presence in patients with painless hematuria: a multicentre study. Eur Urol. 2012 Jan. 61(1):185-92
- Strittmatter F, Buchner A, Karl A, Sommer ML, Straub J, Tilki D, et al. Individual learning curve reduces the clinical value of urinary cytology. Clin Genitourin Cancer. 2011 Sep. 9(1):22-6.
- Babjuk M, Burger M, Zigeuner R, Shariat SF, van Rhijn BW, Compérat E, et al. EAU guidelines on non-muscle-invasive urothelial carcinoma of the bladder: update 2013. Eur Urol. 2013 Oct. 64 (4):639-53.
- NCCN Clinical Practice Guidelines in Oncology. Bladder Cancer. National Comprehensive Cancer Network. Available at http://www.nccn.org/professionals/physician_gls/pdf/bladder.pdf. Version 5.2018 — July 3, 2018; Accessed: August 16, 2018.
- Ehdaie B, Maschino A, Shariat SF, Rioja J, Hamilton RJ, Lowrance WT, et al. Comparative outcomes of pure squamous cell carcinoma and urothelial carcinoma with squamous differentiation in patients treated with radical cystectomy. J Urol. 2012 Jan. 187(1):74-9.
